
THANK YOU FOR JOINING US!
The McMaster Midwifery Research Centre presented the 2022 McMaster Midwifery Research Symposium online over five days from Monday, March 28 to Friday, April 1, 2022 from 12-1330h EST (1600h GMT), that included 1 student research showcase, 2 panel discussions, 3 keynote lectures, 4 research showcases, 5 days, and 6 student research posters.
Registration is now finished at https://tinyurl.com/3z6a5vxw, that had one registration link for any or all days for anyone to attend for free.
Post-Symposium Feedback: Please help us improve the symposium for next year by providing your feedback. The survey is anonymous, unless you indicate your email address for the purpose of receiving a Symposium Certificate of Attendance that will be emailed to you. You can provide your feedback here: https://forms.gle/Sj22i31joGqiojEN9.
You can find below our symposium programme, video presentations, speaker bios, lecture descriptions, and student posters.
Thank you to our panel co-hosts, the National Aboriginal Council of Midwives (NACM), and the Global Network of WHO Collaborating Centers for Nursing and Midwifery (GNWHOCC).
Thank you to all our 31 speakers and 170 symposium participants, that joined us from across Canada and from 28 countries, including: Zimbabwe, Zambia, Virgin Islands (British), United States, United Arab Emirates, Trinidad and Tobago, Thailand, Suriname, South Africa, Somalia, Singapore, Saudi Arabia, Saint Vincent and the Grenadines, Saint Lucia, Saint Barthélemy, Myanmar, Montserrat, Mexico, Japan, Jamaica, India, Hong Kong SAR, Ghana, Egypt, Chile, Canada, Brazil, and Antigua and Barbuda, and 65 Canadian cites: Abbotsford, Acton, Arnprior, Ashton, Barrie, Belleville, Binbrook, Bowmanville, Bracebridge, Brampton, Burlington, Caledon, Calgary, Cambridge, Coldwater, Cole Harbour, Duncan, Edmonton, Elora, Fredericton, Gander, Gatineau, Greater Sudbury, Guelph, Hagersville, Haliburton, Halifax, Hamilton, Ilderton, Kelowna, Kingston, Kitchener, Langley, Lethbridge, L’île-errot, London, Markham, Mississauga, Montreal, Nelson, Niagara on the Lake, North York, Novi, Oakville, Ohsweken, Oshawa, Ottawa, Paris, Québec, Sackville, Sarnia, Scarborough, St. Jacobs, St-Sévère, Sudbury, Surrey, Terrace, Thunder Bay, Toronto, Trois-Rivières, Vancouver, Victoria, Waterloo, Williams Lake, and Winnipeg.
Join us in spring 2023 for the next MMRC Midwifery Research Symposium!
Follow us on social media @macmidwifery on Twitter https://twitter.com/macmidwifery and Facebook https://www.facebook.com/MacMidwifery/!
Sincerely,
Dr. Beth Murray-Davis, Scientific Director
Dr. Liz Darling, Scientist
Prof. Eileen K. Hutton, Scientist
Rashid Ahmed, Research Manager and Symposium Coordinator
McMaster Midwifery Research Centre
Symposium Programme
Register here: https://tinyurl.com/3z6a5vxw
Each day has different events, from Monday, March 28 to Friday, April 1, 1200-1330h EST – please see programme. Register for any one or all days – one Zoom link will be provided.

Post-Symposium Feedback: Please help us improve the symposium for next year by providing your feedback. The survey is anonymous, unless you indicate your email address for the purpose of receiving a Symposium Certificate of Attendance that will be emailed to you. You can provide your feedback here.
Sessions
|
Dr. Giulia Muraca – Safety of forceps and vacuum birth in Canada: from inter-hospital to international perspectives |
Keynote Speaker Thursday, March 31, 2022 – 1200h Dr. Giulia MuracaAssistant Professor, Department of Obstetrics & Gynecology and Department of Health Research Methods, Evidence, and Impact, McMaster UniversitySafety of forceps and vacuum birth in Canada: from inter-hospital to international perspectivesKeynote Description: In industrialized settings, where obstetric intervention has increased significantly in recent decades, the discourse surrounding contemporary birth practices is often framed ideologically as a matter of nature versus technology. The rise in cesarean birth, in particular, is at the very centre of this discourse. Only 5% of Canadian individuals has a cesarean birth in the 1960s, but cesarean birth accounts for approximately 28% of births currently. This increase in cesarean birth has occurred concomitantly with a decline in forceps- and vacuum-assisted birth. This inverse relationship has led to recommendations to increase the use of forceps and vacuum as a strategy to reduce cesarean birth. Forceps and vacuum are considered safe if carried out by trained personnel; however, opportunities for training in forceps and vacuum have declined, and the safety of these deliveries given these shifts in practice warrants inquiry. Using population-based data across Canada, we will explore the trends and comparative outcomes among these modes of birth, quantify population-level impacts, and investigate the safety of these births in hospitals across Canada, with special emphasis on the incidence of maternal and neonatal trauma. CIHR Team for Improving Perinatal Health Care Regionalization in Canada Project website: https://phsr.obgyn.ubc.ca/operative-vaginal-delivery/. Recent publication of this work: https://www.cmaj.ca/content/194/1/E1. |
|
Dr. Rohan D’Souza – Should all pregnant individuals be induced at 39 weeks of gestation? |
Keynote Speaker Friday, April 1, 2022 – 1200h Dr. Rohan D’Souza Associate Professor, Department of Obstetrics & Gynecology and Department of Health Research Methods, Evidence, and Impact, McMaster University Should all pregnant individuals be induced at 39 weeks of gestation? Keynote Description: The proportion of induced labours has increased globally, over the past few decades. Randomized trials comparing labour induction versus expectant management in various populations suggest that inducing labour may reduce caesarean rates and some pregnancy complications. These findings have resulted in changes to recommendations by some organizations, in favour of inducing labour around 39 weeks of gestation, not only for at-risk populations but also, in the absence of medical indications. In this keynote presentation, the speaker will summarize the evidence surrounding labour induction in various populations, present the rationale behind current recommendations and provide suggestions on how shared birthing individuals and families can be supported during the shared decision-making process around the timing of labour induction. |
 |
Panel Discussion
Tuesday, March 29, 2022 – 1200h Co-hosted with the National Aboriginal Council of Midwives (NACM) Finding out what matters to us: The importance of Indigenous-led midwifery research for improving health and well-being Panel Topic Description: A panel discussion with Indigenous midwives and academics on the importance of Indigenous-led midwifery research. The panel will highlight current Indigenous midwifery research projects. We will explore unique approaches to midwifery research and the barriers and facilitating factors for Indigenous midwifery-led research. |
| Watch video on YouTube here: https://www.youtube.com/watch?v=Y1bBufglKcA.
Click Close Captioning (CC) on YouTube screen and use Gear Icon to select available languages for auto-translated subtitles by YouTube. |
Panel Discussion
Wednesday, March 30, 2022 – 1200h Co-hosted with the Global Network of WHO Collaborating Centers for Nursing & Midwifery, Midwifery Network Webinar Global perspectives on the role of midwives in safe abortion care Panel Topic Description: This webinar will be a panel discussion with midwives from around the globe and will explore the role of midwives in ensuring access to safe abortion. Panelists will share their insights and experiences related to training midwives to provide post-abortion care, models of midwifery provision of abortion care, and the potential contributions of midwives towards ensuring access to safe abortion care. |
 |
MMRC Research Showcase
Monday, March 28, 2022 – 1240h Dr. Liz Darling Associate Professor, Department of Obstetrics & Gynecology, McMaster University Ontario midwives’ mental wellbeing: a mixed methods study of barriers and facilitators Project Description: This presentation will share research commissioned by the Association of Ontario Midwives to inform recommendations regarding policy and program level interventions to support improved mental health for midwives in Ontario. We used mixed methods research to identify factors contributing to and negatively impacting Ontario midwives’ mental health, including the experience of racism and bullying in their professional work. The presenter will share an overview of the research findings and recommendations. |
|
Lisa Nussey – Responsibility and justice: Considerations for increasing access to prenatal care |
MMRC Student Showcase
Monday, March 28, 2022 – 1300h Lisa Nussey Health Research Methodology graduate student, McMaster University Responsibility and justice: Considerations for increasing access to prenatal care Project Description: Despite a publicly funded health care system in Canada, disparities in access to prenatal care (PNC) are longstanding and consequential, both clinically and socially. Much is known about the barriers to PNC and client experiences of inadequate PNC (IPNC). However, little is known about care provider perspectives of IPNC, what should be done about it and why we haven’t done it. This presentation will summarize the findings of Nussey’s masters research exploring health and social service provider experiences and understandings of IPNC. Highlights of recommendations for program development to meet the needs of people who struggle to access PNC, including the potential applicability of the concept of Community Centred Care (CCC) will be shared. Nussey will also touch on some preliminary ideas about these provider understandings as they relate to the Social Determinants of Health, mirrored in conceptions of IPNC in the health services literature, obscure the root causes of disparities in access and warrant future consideration. |
|
Dr. Beth Murray-Davis – Making space for midwifery in the hospital: Exploring the birth environment of Canada’s first Alongside Midwifery Unit |
MMRC Research Showcase
Thursday, March 31, 2022 – 1240h Dr. Beth Murray-Davis Associate Professor, Department of Obstetrics & Gynecology, McMaster University Making space for midwifery in the hospital: Exploring the birth environment of Canada’s first Alongside Midwifery Unit Project Description: This study used mixed methods research, underpinned by a socio-spatial framework to explore the impact of the built environment of Canada’s first Alongside Midwifery Unit from the perspective of both midwives and birthing people. Our aim was to assess the impact of the physical environment, and to understand the meanings that individuals attributed to it while also exploring how this influences satisfaction with birth space. The findings revealed that the intentional design elements of the unit facilitated positive experiences and contributed to high levels of satisfaction with the birth experience. We attributed these positive experiences to three key ways of ‘Making Space’ for midwifery-led birth—creating a domestic space in an institutional setting, shifting the technological approach, and sharing ownership of the AMU. The domestic environment was relaxing and comfortable for those in labour, while still maintaining proximity to emergency care. The retooling of the space to support midwifery equipment and resources reinforced midwifery approaches to care and encouraged flexibility, options, and choice for those giving birth. Finally, the built environment led to a greater sense of ownership for all those giving and receiving care. This sense of ownership went beyond the space and how it was designed to include how it was used by midwives, birthing people, and their families. |
|
Allison Guitor – Baby & Mi project: Capturing antibiotic resistance genes in the gut microbiome reveals new benefits of probiotic supplementation in preterm infants |
MMRC Research Showcase Thursday, March 31, 2022 – 1300h Dr. Allison Guitor PhD Candidate, Department of Biochemistry and Biomedical Sciences, McMaster University Baby & Mi project: Capturing antibiotic resistance genes in the gut microbiome reveals new benefits of probiotic supplementation in preterm infants Project Description: Probiotic supplementation is a promising intervention to reduce the impacts of early birth and early antibiotic exposure on the preterm gut microbiome. We hypothesized that early colonization of probiotic strains in preterm infants reduces the abundance of multi-drug resistant bacteria in the gut and their associated antibiotic resistance genes (ARGs). Our study included 13 preterm infants, eight preterm infants that received the probiotic FloraBABY while in-hospital, and nine full term infants from the Baby and PreMi and Baby and Mi studies. We used a targeted capture method to enrich and sequence ARGs from stool samples taken in-hospital and at follow-up visits up to 5 months corrected age from these infants. We identified over 100 ARGs that were unique to infants that did not receive the probiotic. Many ARGs were retained up to 5 months of age and only in the infants not supplemented with probiotics. This pilot survey suggests that probiotics reduce ARGs of clinical concern in the preterm infant gut microbiome, particularly up to 5 months after antibiotic exposure. |
|
Katelyn Fisher, Lauren Columbus, Meagan Furnivall – Framework for a midwifery-led implementation of oxytocin training |
Clinical Practice Showcase Friday, April 1, 2022 – 1240h Katelyn Fisher, Lauren Columbus, Meagan Furnivall Department of Midwifery Leadership Team, London Health Sciences Centre Framework for a midwifery-led implementation of oxytocin training Project Description: The Department of Midwifery Leadership Team at London Health Sciences Centre designed and implemented an oxytocin training program, as well as conducted the evaluation of the program, in response to the need to have all Registered Midwives managing oxytocin according to a standardized protocol. Following the completion of this training program, the leadership created a framework that may assist other midwifery departments in designing, implementing, and evaluating their own training programs for a variety of new clinical skills, such as oxytocin management. The framework includes logistical, leadership, and educational components, including high-fidelity simulation education. |
Student Research Posters
Please scroll down to view all posters.
Graduate and undergraduate students working with Scientists at the McMaster Midwifery Research Centre present their research through posters. Posters are available below. Please help support midwifery research students by viewing their posters.
Congratulations to Claire Ramlogan-Salanga who was awarded Best Symposium Poster by a panel of MMRC adjudications for “Transforming the Midwifery Education Program through social justice curriculum: a modified Delphi study”.
Thank you to all students for their excellent posters and presentations!
Speaker Bios & Lecture Descriptions
- Overview: Three leading researchers present their recent work on prescient topics for midwives.
 |
Dr. Hamideh Bayrampour
Assistant Professor, Midwifery Program, Department of Family Practice, University of British Columbia Perinatal outcomes of planned home birth after cesarean and planned hospital vaginal birth after cesarean at term gestation in British Columbia Monday, March, 28, 2022 – 1200h Lecture Description: In this presentation, perinatal outcomes of planned home birth after cesarean and planned hospital vaginal birth after cesarean among 4,741 midwifery clients with at least one prior cesarean birth are reported. Bio: Dr. Bayrampour has a BSc degree in Midwifery (1999) and a Master’s degree in Midwifery Education (2002) from Iran. Dr Bayrampour earned her PhD in Applied Health Sciences from the University of Manitoba (2012) with a focus on pregnancy at advanced maternal age and completed her postdoctoral studies in the Department of Paediatrics at the University of Calgary (2015) focused on perinatal mental health. Dr Bayrampour joined Midwifery program at UBC in September 2015. Dr. Bayrampour is also an associate member in the School of Population and Public Health and a faculty member in Reproductive and Developmental Sciences program at the University of British Columbia. Dr Bayrampour’s research interests are in the areas of maternal mental health and pregnancy outcomes. She is particularly interested in maternal anxiety and its assessment and management during the perinatal period. She has research expertise in conducting systematic reviews, quantitative and qualitative research, mixed methods studies, and concept analysis. Research Links: https://midwifery.ubc.ca/research/perinatal-wellbeing-research-team/meet-our-team/, |
 |
Dr. Giulia Muraca
Assistant Professor, Department of Obstetrics & Gynecology and Department of Health Research Methods, Evidence, and Impact, McMaster University Safety of forceps and vacuum birth in Canada: From inter-hospital to international perspectives Thursday, March 31, 2022 – 1200h Lecture Description: In industrialized settings, where obstetric intervention has increased significantly in recent decades, the discourse surrounding contemporary birth practices is often framed ideologically as a matter of nature versus technology. The rise in cesarean birth, in particular, is at the very centre of this discourse. Only 5% of Canadian individuals has a cesarean birth in the 1960s, but cesarean birth accounts for approximately 28% of births currently. This increase in cesarean birth has occurred concomitantly with a decline in forceps- and vacuum-assisted birth. This inverse relationship has led to recommendations to increase the use of forceps and vacuum as a strategy to reduce cesarean birth. Forceps and vacuum are considered safe if carried out by trained personnel; however, opportunities for training in forceps and vacuum have declined, and the safety of these deliveries given these shifts in practice warrants inquiry. Using population-based data across Canada, we will explore the trends and comparative outcomes among these modes of birth, quantify population-level impacts, and investigate the safety of these births in hospitals across Canada, with special emphasis on the incidence of maternal and neonatal trauma. CIHR Team for Improving Perinatal Health Care Regionalization in Canada Project website: https://phsr.obgyn.ubc.ca/operative-vaginal-delivery/. Recent publication of this work: https://www.cmaj.ca/content/194/1/E1. Bio: Dr. Giulia Muraca is a perinatal epidemiologist and an Assistant Professor in the Departments of Obstetrics and Gynecology and Health Research Methods, Evidence & Impact at McMaster University. Dr. Muraca’s research program aims to use population-based database linkages and epidemiologic approaches to support enhanced safety and satisfaction in the care of pregnant individuals and their children, with emphasis on care quality, accessibility and equity. Contact: muracag@mcmaster.ca. |
 |
Dr. Rohan D’Souza
Associate Professor, Department of Obstetrics & Gynecology and Department of Health Research Methods, Evidence, and Impact, McMaster University Should all pregnant individuals be induced at 39 weeks of gestation?
Friday, April 1, 2022 – 1200h Keynote Description: The proportion of induced labours has increased globally, over the past few decades. Randomized trials comparing labour induction versus expectant management in various populations suggest that inducing labour may reduce caesarean rates and some pregnancy complications. These findings have resulted in changes to recommendations by some organizations, in favour of inducing labour around 39 weeks of gestation, not only for at-risk populations but also, in the absence of medical indications. In this keynote presentation, the speaker will summarize the evidence surrounding labour induction in various populations, present the rationale behind current recommendations and provide suggestions on how shared birthing individuals and families can be supported during the shared decision-making process around the timing of labour induction.Bio: Rohan D’Souza MD PhD FRCOG is an Associate Professor with the Departments of Obstetrics & Gynaecology and Health Research Methods, Evidence & Impact at McMaster University, Hamilton. His clinical and research interests, include reducing maternal morbidity, improving pregnancy outcomes for individuals with medical conditions, optimizing the success and safety of labour induction and incorporating preferences of pregnant individuals into clinical decision-making. His ongoing research projects include establishing a Canada-wide obstetric surveillance system (CanOSS) for severe maternal morbidity, increasing COVID-19 vaccine confidence among pregnant and postpartum Canadians (The Confidence Project), preventing postpartum haemorrhage and improving outcome selection and reporting in pregnancy studies. |
Overview: A panel discussion with Indigenous midwives and academics on the importance of Indigenous-led midwifery research. The panel will highlight current Indigenous midwifery research projects. We will explore unique approaches to midwifery research and the barriers and facilitating factors for Indigenous midwifery-led research. Panel is co-hosted by the National Aboriginal Council of Midwives.

 |
Claire Dion Fletcher
RM, Co-Chair, National Aboriginal Council of Midwives (NACM) Panel moderator Finding out what matters to us: The importance of Indigenous-led midwifery research for improving health and well-being Bio: Claire Dion Fletcher (she/her) is a Lenape- Potawatomi and mixed settler Registered Midwife practicing at Seventh Generation Midwives Toronto. She is presently co-chair of the National Aboriginal Council of Midwives and Assistant Professor at the Ryerson Midwifery Education Program in Toronto. Her teaching focuses on Indigenous midwifery and social justice issues. Claire is deeply committed to increasing diversity in the midwifery profession through Indigenous-led education. She completed her Master of Arts in Gender, Feminist and Women’s Studies at York University where her research focused on decolonized health care and Indigenous midwifery. Claire is committed to reproductive justice and Indigenous feminisms and how these frameworks shape midwifery education and practice. She is an adoring Auntie to her niece and nephews. |
 |
Cheryllee Bourgeois
Métis Midwife Panelist Finding out what matters to us: The importance of Indigenous-led midwifery research for improving health and well-being Bio: Tansi Nitotemtek! My name is Cheryllee Bourgeois, I am a Metis midwife and follow Cree / Metis teachings in line with my ancestry from the Red River District in southern Manitoba and North Dakota. I have been a midwife here since 2007 and helped to develop and set up Seventh Generation Midwives Toronto (SGMT) when I was a student midwife at Ryerson. I worked as a Registered Midwife for 11 years before give-up my registration in 2018 to work under the exemption clause, which is unique at SGMT. This means that I am able to provide care in line with needs identified by the Indigenous community in Toronto. I provide sexual and reproductive health care through the life cycle and I am very committed to both increasing access to Indigenous focused health care and supporting more Indigenous folks to become midwives. I am very grateful to live and work in the Dish with One Spoon territory as a midwife and to raise my three kids here. |
| Carol Couchie
Nishnawbe Midwife Panelist Finding out what matters to us: The importance of Indigenous-led midwifery research for improving health and well-being Bio: Carol Couchie is a Nishnawbe Kwe from Nipissing First Nation. She is a mother and grandmother, and has worked as a Midwife for 20 years in Ontario, Northern Manitoba and Northern Quebec. She has attended upwards of 800 births in her work as a midwife. She is one of the original members of the National Aboriginal Council of Midwives, and she is currently the NACM Mentorship and Resilience lead. She now lives in her home community of Nipissing First Nation where she helped found KTigaaning Midwives, an Indigenous focused Midwifery practice and Birth Center with her daughter Rachel Dennis-Couchie. |
 |
Dr. Karen Lawford Assistant Professor, Department of Gender Studies, Queen’s University Aboriginal midwife, Namegosibiing, Lac Seul First Nation, Treaty 3, and Registered midwife (Ontario) Panelist Finding out what matters to us: The importance of Indigenous-led midwifery research for improving health and well-being Bio: Dr. Lawford is an Aboriginal midwife (Namegosibiing, Lac Seul First Nation, Treaty 3) and a Registered midwife (Ontario). Her research focuses on comprehensive, gender-inclusive sexual and reproductive healthcare for Indigenous Peoples with a particular focus on the provision of maternity care for those who live on reserve. Dr. Lawford seeks to identify the barriers to achieving equitable health services for Indigenous Peoples. She was the 2020 Indspire Laureate in Health for her research and policy work on mandatory evacuation for birth. Her research interests also include Maternity care on reserves, Medical evacuation, Midwifery, Indigenous feminist theories and methodologies, Indigenous women and Two Spirit Leadership, Indigenous health and wellness, and Health care. She is an Assistant Professor in the Department of Gender Studies at Queen’s University, and affiliated with the Queen’s Cultural Studies Interdisciplinary Graduate Program, and holds an Adjunct Research Professor position with the School of Indigenous and Canadian Studies at Carleton University. More info: https://www.queensu.ca/gnds/people/karen-lawford |
 |
Dr. Jennifer Leason
Off-reserve member of Pine Creek Indian Band, Manitoba Associate Professor, Department of Anthropology and Archaeology, University of Calgary Canada Research Chair, Tier II, Indigenous Maternal Child Wellness Panelist Finding out what matters to us: The importance of Indigenous-led midwifery research for improving health and well-being Bio: Boozhoo, Aniin Keesis Sagay Egette Kwe nindiznikaaz. Dr. Jennifer Leason (she/he/kwé pronouns) is an off-reserve member of Pine Creek Indian Band, Manitoba and the proud mother of Lucas and Lucy. Dr. Leason is a Canadian Institute of Health Research (CIHR), Canada Research Chair, Tier II, Indigenous Maternal Child Wellness and an Associate Professor at the University of Calgary. Dr. Leason is an Associate Member of the CIHR College of Reviewers and serves on the Institute of Indigenous Peoples Health Advisory Board. She is an Associate Editor of the Canadian Journal of Public Health and member of the Canadian Perinatal Surveillance System with the Public Health Agency of Canada. Her research aims to address perinatal and maternal-child health disparities and inequities by examining maternity experiences, healthcare utilization, and social-cultural contexts of Indigenous maternal child wellness. |
This webinar will be a panel discussion with midwives from around the globe and will explore the role of midwives in ensuring access to safe abortion. Panelists will share their insights and experiences related to training midwives to provide post-abortion care, models of midwifery provision of abortion care, and the potential contributions of midwives towards ensuring access to safe abortion care.
For more info on the Global Network of WHO Collaborating Centers for Nursing & Midwifery (GNWHOCC), visit https://globalnetworkwhocc.com/
Related links to panel discussion:
1. Article mentioned in panel discussion: “Midwives and post-abortion care in Gabon: ‘Things have really changed’” / «Les sages-femmes et les soins après avortement au Gabon: «Les choses ont vraiment changé»» by/par: Aimée Patricia Ndembi Ndembi, Justine Mekuí, Gail Pheterson, Marijke Alblas. Published in the Health and Human Rights Journal, Special Section on Abortion Law Reform, Volume 21, December 2019.
In English: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2469/2019/12/Pheterson.pdf
2. Both panelists Marina Baig and Arusa Lakhani co-authored an e-book in 2020 with the MMRC’s Professors Karyn Kaufman and Eileen Hutton entitled “Woman-Centered Reproductive Health Care: An e-Resource for Lady Health Visitors & Midwives in Pakistan”, available for free pdf download at: https://www.radixantiqua.com/product/free-e-book-for-midwives/.

 |
Cristina Alonso
Consultant to the American College of Nurse Midwives Panelist Global perspectives on the role of midwives in safe abortion care Bio: Cristina has dedicated her career to ensuring access to quality sexual and reproductive health services in Central America and Mexico. Cristina worked in Honduras, Guatemala and Costa Rica providing services and training midwives and physicians on safe and respectful birth, abortion, family planning and sexual health with Marie Stopes International and other local NGOs. After completing her MPH at Tulane University, she moved to Mexico in 2003 where she founded the Luna Maya birth centers in Chiapas and Mexico City. She was a founding member and President of the Mexican Midwifery Association from 2014 to 2017 and has collaborated extensively with the International Confederation of Midwives (ICM) and UNFPA. She has worked with several international networks and the World Health Organization to create a global definition and standards for Midwifery Centers. She founded the Mexican Network of Midwifery Centers and created an e-learning program with a manual on “How to Open a Birth Center” directed at improving respectful care and birth outcomes in Mexico and Latin America. |
 |
Marina Baig
Senior Instructor and Head of Maternal, Newborn, Child Health and Midwifery Stream, Aga Khan University School of Nursing and Midwifery, Karachi, Pakistan Panelist Global perspectives on the role of midwives in safe abortion care Bio: Marina Baig Hashwani does research in midwifery education and practice, capacity building of midwives and other midlevel providers, family planning and post-abortion care, and maternal and newborn care. Her recent publications include “Induced abortions in Pakistan: an afflicting challenge needing addressal” in the British Journal of Midwifery in February 2022. |
 |
Arusa Lakhani
Assistant Professor, Aga Khan University School of Nursing and Midwifery, Karachi, Pakistan Panelist Global perspectives on the role of midwives in safe abortion care Bio: Arusa completed her Masters in Nursing in 2007 and currently is a PhD scholar doing her research in the area of children with intellectual disabilities. She has more than 25 years of experience in teaching nursing and midwifery students. At the national level, she has participated actively in developing midwifery and nursing curriculums and extensive experience in leading several workshops and sessions. Internationally, she has worked in developing nursing and midwifery curriculum for the AKU East Africa and Afghanistan. Her most appreciated contribution in the field of Midwifery along with her team is the creation of the first undergraduate midwifery program in Pakistan – the first of its kind in South Asia.. She is also the current President of the Midwifery Association of Pakistan. She has conducted several research studies, national and international training in midwifery, and received grants in the MNCH area, supervised thesis for the masters in nursing students, and published articles in the field of Education, midwifery and women’s health. |
 |
Alixandra Bacon
Registered Midwife, and President, Canadian Association of Midwives Panelist Global perspectives on the role of midwives in safe abortion care Bio: Alixandra Bacon is a Registered Midwife and settler living and working in Vancouver, BC on the traditional and unceded territories of the Musqueam, Squamish, Tsleil-waututh and Tsawassen nations. Alix is the President of the Canadian Association of Midwives, Past President of the Midwives Association of BC and clinical faculty with UBC Midwifery. Alix is inspired by the power of midwifery associations to grow and strengthen the workforce, contribute to policy development and promote social accountability to ultimately improve the health, rights and birthing people in Canada and around the world through provision of equitable and respectful care. |
 |
Justine Mekui Ella
Panelist Global perspectives on the role of midwives in safe abortion care Bio: Justine Mekui Ella, is a senior midwife in the outpatient department of the Jeanne EBORI Foundation Mother-Child University Hospital Center (CHUMEFJE) in Libreville, Gabon. Justine is the Medical Coordinator of the Central African Network for Women’s Reproductive Health in Gabon, Cameroon, and Equatorial Guinea, sub-regional trainer in manual intrauterine aspiration (MVA), and does capacity building for midwives in the insertion and removal of implants and IUDs. Justine is co-author of “Midwifery and Post-Abortion Care: Things Have Really Changed.” She contributed with the WHO and the Ministry of Health in the drafting of national guidelines on the management of incomplete abortions in 2021. Her work builds on the capacity of health providers in the management of pregnancy complications in the first trimester in order to fight against maternal morbidity and mortality. She is responsible for family planning at CHUMEFJE, and is an active member of the Association of Midwives of Gabon. email jmekuiella@gmail.com Justine Mekui Ella est sage-femme major au service des consultations externes du Centre Hospitalier Universitaire Mère-Enfant de la Fondation Jeanne EBORI (CHUMEFJE) de Libreville au Gabon. Elle est coordinatrice Médicale du Réseau d’Afrique Centrale pour la santé reproductive des femmes du Gabon, du Cameroun, et de la Guinée Équatoriale, et Formatrice sous régionale à l’aspiration manuelle intra-utérine (AMIU) et au renforcement des capacités des sages-femmes à la pose et au retrait des implants et DIUs. Elle est co-auteure de “Sages-femmes et les soins après avortements: les choses ont vraiment changé.” Elle a contribué avec l’OMS et le Ministère de la santé à la rédaction des directives nationales sur la prise en charge des avortements incomplets en 2021. Elle renforce les capacités des prestataires de soins de santé dans leur prise en charge des complications de la grossesse au premier trimestre afin de lutter contre la morbide-mortalité maternelle. Elle est responsable de la planification familiale au CHUMEFJE, et membre active de l’association des sages-femmes du Gabon. e-mail jmekuiella@gmail.com |
 |
Marijke Alblas
Panelist Global perspectives on the role of midwives in safe abortion care Bio: Marijke Alblas is a medical doctor, specialised in SRHR, mainly working as a second trimester abortion provider and abortion trainer of doctors, nurses and midwives in South Africa, where abortion was legalised in 1996. She has been involved in several abortion projects in other countries, one of them on the North East Caribbean islands, but especially the training of midwives in Post Abortion Care with the Middle Africa Network for Women’s Reproductive Health: Gabon, Cameroon, Equatorial Guinee (GCG) that was successful in showing that midwives when trained properly in PAC can save women’s lives |
 |
Aimée Patricia Ndembi
Panelist Global perspectives on the role of midwives in safe abortion care Bio: Aimée Patricia Ndambi is a clinical psychologist and researcher in the Department of Research on Social Dynamics (DRDS) at IRSH-CENAREST in Gabon. Her research focuses on sexual and reproductive health and generational transmission. She co-wrote “Midwives and Post-Abortion Care in Gabon: Things have really changed” in the Health and Human Rights Journal in 2019. She also participated in the book “Faire Sortir la Grossesse – Savoirs, itinéraires et protocoles autour de l’avortement en Afrique subsaharienne” (“Getting the pregnancy out: Knowledge, itineraries and protocols related to abortion in sub-Saharan Africa”) published by L’Harmattan in 2022. She is the co-founder and president of the Central African Network for Women’s Reproductive Health for Gabon, Cameroon, and Equatorial Guinea. Aimée Patricia Ndembi est Psychologue clinicienne et chercheure au Département de recherche sur les dynamiques sociales (DRDS) de l’IRSH-CENAREST au Gabon. Ses recherches portent sur la santé sexuelle et reproductive et sur les transmissions générationnelles. Elle est co-auteure de «Midwives and Post-Abortion Care in Gabon: Things have really changed» («Les Sages-Femmes et les Soins Post-Avortement au Gabon: Les Chose Ont Vraiment Changé») dans Health and Human Rights Journal en 2019. Elle a participé également à l’ouvrage «Faire Sortir la Grossesse – Savoirs, itinéraires et protocoles autour de l’avortement en Afrique subsaharienne» chez L’Harmattan en 2022. Elle est la co-fondatrice et la présidente du Réseau d’Afrique Centrale pour le Santé Reproductive des Femmes pour le Gabon, le Cameroun, et la Guinée-Equatoriale. |
- Overview: Midwifery and related research scholars present their work on a variety of topics, approaches, and methods highlighting research being done at the McMaster Midwifery Research Centre, McMaster University, and London Health Sciences Centre.
 |
Dr. Liz Darling
Ontario midwives’ mental wellbeing: a mixed methods study of barriers and facilitators Monday, March 28, 2022 – 1240h Bio: Dr. Liz Darling, BArtsSc, BHSc, MSc, PhD, is a Registered Midwife, Assistant Dean and Director of the Midwifery Education Program, Associate Professor in the Department of Obstetrics and Gynecology, an Adjunct Scientist at the Institute for Clinical Evaluative Sciences, and an Associate with the Department of Health Research Methods, Evidence, and Impact at McMaster University. She is the principal investigator on a CIHR Early Career Operating Grant in Maternal, Reproductive, Child, and Youth Health. Her current research interests include: the organization of midwifery services, health disparities, access to care, health policy, and perinatal health surveillance. She conducts mixed methods research and has particular expertise in the midwifery data collected in Ontario’s perinatal registry (BORN-Ontario). Contact: darlinek@mcmaster.ca Project Description: This presentation will share research commissioned by the Association of Ontario Midwives to inform recommendations regarding policy and program level interventions to support improved mental health for midwives in Ontario. We used mixed methods research to identify factors contributing to and negatively impacting Ontario midwives’ mental health, including the experience of racism and bullying in their professional work. The presenter will share an overview of the research findings and recommendations. |
 |
Lisa Nussey
Responsibility and justice: Considerations for increasing access to prenatal care Monday, March 28, 2022 – 1300h Bio: Lisa Nussey is a registered midwife in Hamilton. She recently completed a Masters in the Health Research Methods program at McMaster University. She is the founder and co-coordinator of the Hamilton Midwifery Outreach Team (HMOT), a group of volunteer midwives providing low barrier prenatal care to people in the shelter system in Hamilton. She works with the Hamilton Social Medicine Response Team (HAMSMaRT), a grass roots, interdisciplinary health organization providing low barrier health care to people in Hamilton. HAMSMaRT works to promote the idea that health is political and that only through social transformation can barriers to health and health care truly be addressed. Lisa served on the College of Midwives of Ontario’s Council and Investigations, Complaints and Reports Committee from 2017 to 2020. Lisa’s primary areas of interest are Community Centred Care, the Social Determination of Health and Social Medicine. Project Description: Despite a publicly funded health care system in Canada, disparities in access to prenatal care (PNC) are longstanding and consequential, both clinically and socially. Much is known about the barriers to PNC and client experiences of inadequate PNC (IPNC). However, little is known about care provider perspectives of IPNC, what should be done about it and why we haven’t done it. This presentation will summarize the findings of Nussey’s masters research exploring health and social service provider experiences and understandings of IPNC. Highlights of recommendations for program development to meet the needs of people who struggle to access PNC, including the potential applicability of the concept of Community Centred Care (CCC) will be shared. Nussey will also touch on some preliminary ideas about these provider understandings as they relate to the Social Determinants of Health, mirrored in conceptions of IPNC in the health services literature, obscure the root causes of disparities in access and warrant future consideration. |
 |
Dr. Beth Murray-Davis
Making space for midwifery in the hospital: Exploring the birth environment of Canada’s first Alongside Midwifery Unit Thursday, March 31, 2022 – 1240h Bio: Dr. Beth Murray-Davis, BA, BHSc, MA, PhD, RM, is an Associate Professor in the Midwifery Education Program and Department of Obstetrics and Gynecology. She is a co-PI for a CIHR Clinician Investigator Team Grant examining Non-Communicable Diseases in Obstetrics. Her current research interests include pregnant peoples’ experiences of healthy nutrition and exercise during pregnancy and postpartum, fetal movement awareness, midwifery experiences of caring for complicated pregnancies, client and health care provider experiences of alternative models of practice for midwives, and client decision making about place of birth. Dr. Murray-Davis has worked as a midwife in Hamilton since 2003. Contact: bmurray@mcmaster.ca. Project Description: This study used mixed methods research, underpinned by a socio-spatial framework to explore the impact of the built environment of Canada’s first Alongside Midwifery Unit from the perspective of both midwives and birthing people. Our aim was to assess the impact of the physical environment, and to understand the meanings that individuals attributed to it while also exploring how this influences satisfaction with birth space. The findings revealed that the intentional design elements of the unit facilitated positive experiences and contributed to high levels of satisfaction with the birth experience. We attributed these positive experiences to three key ways of ‘Making Space’ for midwifery-led birth—creating a domestic space in an institutional setting, shifting the technological approach, and sharing ownership of the AMU. The domestic environment was relaxing and comfortable for those in labour, while still maintaining proximity to emergency care. The retooling of the space to support midwifery equipment and resources reinforced midwifery approaches to care and encouraged flexibility, options, and choice for those giving birth. Finally, the built environment led to a greater sense of ownership for all those giving and receiving care. This sense of ownership went beyond the space and how it was designed to include how it was used by midwives, birthing people, and their families. |
 |
Allison Guitor
Capturing antibiotic resistance genes in the gut microbiome reveals new benefits of probiotic supplementation in preterm infants Thursday, March 31, 2022 – 1300h Bio: Allison completed her BSc in Biology at the University of Waterloo. During her undergraduate co-op program, she worked for various government agencies and as a research assistant in Dr. Lynne Howell’s lab at the University of Toronto. After graduation, Allison joined Dr. Gerry Wright’s group as a Master’s student and later decided to pursue her PhD studies there as well. Allison’s project focuses on developing and implementing sequencing-based technology to enrich our understanding of antibiotic resistance in the gut microbiome after various perturbations including antibiotic and probiotic use. Contact: guitora@mcmaster.ca Project Description: Probiotic supplementation is a promising intervention to reduce the impacts of early birth and early antibiotic exposure on the preterm gut microbiome. We hypothesized that early colonization of probiotic strains in preterm infants reduces the abundance of multi-drug resistant bacteria in the gut and their associated antibiotic resistance genes (ARGs). Our study included 13 preterm infants, eight preterm infants that received the probiotic FloraBABY while in-hospital, and nine full term infants from the Baby and PreMi and Baby and Mi studies. We used a targeted capture method to enrich and sequence ARGs from stool samples taken in-hospital and at follow-up visits up to 5 months corrected age from these infants. We identified over 100 ARGs that were unique to infants that did not receive the probiotic. Many ARGs were retained up to 5 months of age and only in the infants not supplemented with probiotics. This pilot survey suggests that probiotics reduce ARGs of clinical concern in the preterm infant gut microbiome, particularly up to 5 months after antibiotic exposure. |

|
Katelyn Fisher, RM; Lauren Columbus, RM; Meagan Furnivall, RM
Department of Midwifery Leadership Team, London Health Sciences Centre Framework for a Midwifery-led implementation of oxytocin Friday, April 1, 2022 – 1240h Bios: Katelyn Fisher is a Registered Midwife with Midwives of Middlesex & Area, and the Chief of the Department of Midwifery at LHSC. Her current research involves exploring interprofessional work and collaboration between midwives and pediatricians. Lauren Columbus is a Registered Midwife with Midwives of Middlesex & Area, and the Academic Practice Lead in the Department of Midwifery at LHSC. She is a current graduate student at the School of Health Professions Education at Maastricht University. Her research interests include interprofessional communication and team dynamics, best practice in fetal health surveillance, and simulation. Meagan Furnivall is a Registered Midwife with Talbot Creek Midwives, and the Department Research Lead. Her research interests include skin-to-skin contact in cesarean section, shared decision-making, postpartum mental illness and midwifery burn out. Contact: katelyn.fisher@lhsc.on.ca, lauren.columbus@lhsc.on.ca, meagan.furnivall@lhsc.on.ca Project Description: The Department of Midwifery Leadership Team at London Health Sciences Centre designed and implemented an oxytocin training program, as well as conducted the evaluation of the program, in response to the need to have all Registered Midwives managing oxytocin according to a standardized protocol. Following the completion of this training program, the leadership created a framework that may assist other midwifery departments in designing, implementing, and evaluating their own training programs for a variety of new clinical skills, such as oxytocin management. The framework includes logistical, leadership, and educational components, including high-fidelity simulation education. |
- Overview: Graduate and undergraduate students working with Scientists at the McMaster Midwifery Research Centre present their research through posters available online during the symposium for your review on our website.
 |
Elizabeth Hilsenteger
Poster Title: The Global Midwifery Peer-to-Peer Program Bio: Elizabeth is a fourth-year Bachelor of Health Science (Honours) student at McMaster University. She is passionate about health and healthcare especially as it intersects with philosophical issues; she hopes to pursue a degree in bioethics and midwifery after completing her BHSc. She is currently conducting research in midwifery education and is part of the McMaster Midwifery Research Centre. Study Description: The Global Midwifery Peer-to-Peer Program aims to connect midwifery students in Australia and Canada to foster conversations that expand sociocultural knowledge and aid in their overall learning. Cultural competence is becoming a requirement of caring professions, especially in the context of global health. Therefore, it is imperative to nurture cultural competence in the education of future midwives. The effectiveness of the collaborative activity will be measured by comparing the results of two surveys; one completed prior to the intervention, and one completed after. Preliminary findings will be shared during the poster presentation as we plan to review the final survey results in early March. |
 |
Emma Ruby
Poster Title: Gestational Diabetes Mellitus Screening and Counselling Practices of Antenatal Healthcare Providers in Ontario: Exploring the Perspectives of Patients Bio: Emma Ruby is a 4th year undergraduate student in the Bachelor of Health Sciences (Honours) Program, within the Child Health Specialization at McMaster University. Her interests lie in improving maternal and infant health outcomes pertaining to non-communicable diseases such as diabetes, obesity, and hypertension, as well as improving care provision throughout the perinatal period. Emma has a well-developed understanding of the social determinants of healthy child development and has more recently expanded this interest to explore how early child development is impacted by maternal experiences throughout the pregnancy period. Currently, Emma is completing her Honours thesis project within the McMaster Midwifery Research Centre under the supervision of Dr. Beth Murray-Davis. Study Description: This qualitative, grounded theory study, aimed to explore the experiences of gestational diabetes mellitus (GDM) screening and counselling practices among antenatal healthcare providers (HCPS) in Ontario, specifically midwives, family physicians, and obstetricians, from the perspectives of patients. This study was conducted in collaboration with the Diabetes, Obesity, and Hypertension in Pregnancy Research Network (DOH-NET) and the Southern Ontario Obstetrical Network (SOON). The goal of this paper was to provide a qualitative analysis, using a patient-centered approach, to explore the impact of variations in screening guidelines and changing patient population trends on GDM care provision. The research team was interested in exploring whether the experiences of patients may inform future research directions or clinical practice guidelines pertaining to GDM screening and counselling. |
 |
Ayeshah Haque
Poster title: Health equity data collection – a survey of Ontario midwives Bio: Ayeshah Haque is a midwife and recently completed her graduate studies in the Translational Research Program at the University of Toronto. She was awarded the AOM Mentored Midwifery Research Grant to identify key factors that would impact implementation. Study Description: Based on her thesis work, this study explored health equity data collection amongst Ontario midwives. |
 |
Claire Ramlogan-Salanga
Poster Title: Transforming the Midwifery Education Program through social justice curriculum: a modified Delphi study Bio: Claire Ramlogan-Salanga is a registered midwife, sessional instructor with the McMaster Midwifery Education Program and current Master’s of Science in Health Education thesis student. She is a recent recipient of the Ontario Graduate Scholarship and the HSED Outstanding Achievement Award from the Faculty of Health Science. Her leadership positions include Chair of Council at the College of Midwives of Ontario and Chair of the Equity, Diversity, and Inclusion Committee of the Canadian Midwifery Regulators Council. An additional contribution to the midwifery community is her development of the Canadian National IBPOC Midwifery Peer Review program that supports community building and information sharing. Her research interests include health education, social justice education reform, intersectional approaches to research design and health equity. Study Description: This study uses a modified Delphi approach, which includes focus groups and interviews with subject matter experts, two rounds of surveys with key informants, and a final member checking session. Participants were recruited through both purposeful and snowball sampling. The Delphi methodology involves an iterative data analysis process, therefore upon completion of each focus group and round of surveys, analysis has been conducted and used to form the following rounds of the Delphi. Qualitative data has undergone primary coding, secondary coding, and then theme formation. Quantitative data has been gathered using REDCap and analyzed using descriptive statistics. Based on the social justice elements identified by participants, development intended learning outcomes will be compared to the national midwifery competencies to determine alignment. Recommendations to the Ontario Midwifery Education Program (OMEP) will be reviewed at a final member checking session. The future implication of this study is the revision of the Midwifery Education Programs curriculum and to provide an example for other Canadian MEPs. The broader implications include integration of social justice curriculum by other Canadian MEPs and other health professions education programs. |
 |
Shikha Gandhi
Poster Title: Identifying Strengths and Gaps in Canadian Midwifery Research: A Scoping Review Bio: Shikha is a fourth-year Honours Life Sciences student at McMaster University, where she is currently conducting her thesis with the McMaster Midwifery Research Centre (MMRC). Over the course of her undergraduate career, Shikha has found a great passion for research and is excited to further the knowledge she has gained thus far. Contact: gandhs15@mcmaster.ca. Study Description: Over the last 25 years, the profession of midwifery has continued to grow rapidly throughout Canada. Research suggests that midwifery-led care has the potential to improve maternal/infant outcomes, improve client satisfaction and increase breastfeeding rates. The purpose of this scoping review was to identify the progress, strengths, gaps, priorities, and directions of midwifery research in the Canadian context to develop resources for registered midwives, midwifery researchers, professional associations, regulatory bodies, and funding agencies. |
 |
Erika Campbell
Poster Title: Opposing oppression within health services for First Nations evacuated out of their community to give birth: A Review of Guidelines, Practices, and Recommendations to Conceptualize Anti-Oppressive Maternity Care Bio: Erika is a PhD candidate in Global Health at McMaster University. Her doctoral research, supervised by Dr. Liz Darling and Dr. Karen Lawford, explores the influence of the dominate western culture within the federal and Ontario healthcare systems related to the provision of maternity care provided to First Nations peoples who are evacuated out of their communities to give birth. She is unsure what she we do after completion of her PhD. However, Erika knows that she wants to contribute as a researcher, educator, and advocate to establishing and maintaining sexual and reproductive healthcare that is accessible and safe for service users. Study Description: Using critical interpretive synthesis, Erika reviewed literature pertaining to guidelines, practices, and recommendations about maternity care for First Nations evacuated from their communities to give birth in hospitals to conceptualize anti-oppressive maternity care practices for care providers serving this patient population. Erika analyzed 63 different documents, from peer reviewed journal articles to gray literature, to thematically organize anti-oppressive practices through the Core Principles of Change of the Calls for Justice from Reclaiming Power and Place: The Final Report of the National Inquiry into Missing and Murdered Indigenous Women and Girls. This review is an ongoing piece of work that is likely to change in the way ideas are communicate, but Erika is grateful to be able to share this work to generate discussion about our collective responsibility to make maternity care anti-oppressive. Erika would like to acknowledge and thank her PhD committee, Dr. Liz Darling, Dr. Bonnie Freeman, and Dr. Karen Lawford, for their insights and feedback throughout the process of conducting this review. |
Student Research Posters
Student Research Posters are available all week for symposium attendees to view. Study descriptions and presenter bios are available below. A panel of adjudicators will present Best Poster award at the conclusion of the symposium on Friday. Please support our students by viewing this interesting and diverse set of research projects!
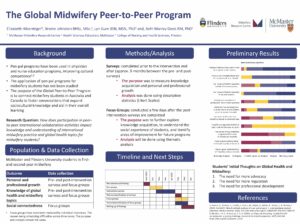
Elizabeth Hilsenteger
Poster Title: The Global Midwifery Peer-to-Peer Program
Bio: Elizabeth is a fourth-year Bachelor of Health Science (Honours) student at McMaster University. She is passionate about health and healthcare especially as it intersects with philosophical issues; she hopes to pursue a degree in bioethics and midwifery after completing her BHSc. She is currently conducting research in midwifery education and is part of the McMaster Midwifery Research Centre.
Study Description: The Global Midwifery Peer-to-Peer Program aims to connect midwifery students in Australia and Canada to foster conversations that expand sociocultural knowledge and aid in their overall learning. Cultural competence is becoming a requirement of caring professions, especially in the context of global health. Therefore, it is imperative to nurture cultural competence in the education of future midwives. The effectiveness of the collaborative activity will be measured by comparing the results of two surveys; one completed prior to the intervention, and one completed after. Preliminary findings will be shared during the poster presentation as we plan to review the final survey results in early March.
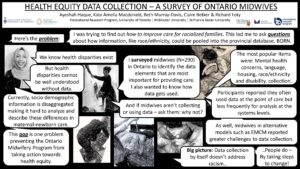
Ayeshah Haque
Poster title: Health equity data collection – a survey of Ontario midwives
Bio: Ayeshah Haque is a midwife and recently completed her graduate studies in the Translational Research Program at the University of Toronto. She was awarded the AOM Mentored Midwifery Research Grant to identify key factors that would impact implementation.
Study Description: Based on her thesis work, this study explored health equity data collection amongst Ontario midwives.

Emma Ruby
Poster Title: Gestational Diabetes Mellitus Screening and Counselling Practices of Antenatal Healthcare Providers in Ontario: Exploring the Perspectives of Patients
Bio: Emma Ruby is a 4th year undergraduate student in the Bachelor of Health Sciences (Honours) Program, within the Child Health Specialization at McMaster University. Her interests lie in improving maternal and infant health outcomes pertaining to non-communicable diseases such as diabetes, obesity, and hypertension, as well as improving care provision throughout the perinatal period. Emma has a well-developed understanding of the social determinants of healthy child development and has more recently expanded this interest to explore how early child development is impacted by maternal experiences throughout the pregnancy period. Currently, Emma is completing her Honours thesis project within the McMaster Midwifery Research Centre under the supervision of Dr. Beth Murray-Davis.
Study Description: This qualitative, grounded theory study, aimed to explore the experiences of gestational diabetes mellitus (GDM) screening and counselling practices among antenatal healthcare providers (HCPS) in Ontario, specifically midwives, family physicians, and obstetricians, from the perspectives of patients. This study was conducted in collaboration with the Diabetes, Obesity, and Hypertension in Pregnancy Research Network (DOH-NET) and the Southern Ontario Obstetrical Network (SOON). The goal of this paper was to provide a qualitative analysis, using a patient-centered approach, to explore the impact of variations in screening guidelines and changing patient population trends on GDM care provision. The research team was interested in exploring whether the experiences of patients may inform future research directions or clinical practice guidelines pertaining to GDM screening and counselling.

Claire Ramlogan-Salanga
Poster Title: Transforming the Midwifery Education Program through social justice curriculum: a modified Delphi study
Bio: Claire Ramlogan-Salanga is a registered midwife, sessional instructor with the McMaster Midwifery Education Program and current Master’s of Science in Health Education thesis student. She is a recent recipient of the Ontario Graduate Scholarship and the HSED Outstanding Achievement Award from the Faculty of Health Science. Her leadership positions include Chair of Council at the College of Midwives of Ontario and Chair of the Equity, Diversity, and Inclusion Committee of the Canadian Midwifery Regulators Council. An additional contribution to the midwifery community is her development of the Canadian National IBPOC Midwifery Peer Review program that supports community building and information sharing. Her research interests include health education, social justice education reform, intersectional approaches to research design and health equity.
Study Description: This study uses a modified Delphi approach, which includes focus groups and interviews with subject matter experts, two rounds of surveys with key informants, and a final member checking session. Participants were recruited through both purposeful and snowball sampling. The Delphi methodology involves an iterative data analysis process, therefore upon completion of each focus group and round of surveys, analysis has been conducted and used to form the following rounds of the Delphi. Qualitative data has undergone primary coding, secondary coding, and then theme formation. Quantitative data has been gathered using REDCap and analyzed using descriptive statistics. Based on the social justice elements identified by participants, development intended learning outcomes will be compared to the national midwifery competencies to determine alignment. Recommendations to the Ontario Midwifery Education Program (OMEP) will be reviewed at a final member checking session. The future implication of this study is the revision of the Midwifery Education Programs curriculum and to provide an example for other Canadian MEPs. The broader implications include integration of social justice curriculum by other Canadian MEPs and other health professions education programs.

Shikha Gandhi
Poster Title: Identifying Strengths and Gaps in Canadian Midwifery Research: A Scoping Review
Bio: Shikha is a fourth-year Honours Life Sciences student at McMaster University, where she is currently conducting her thesis with the McMaster Midwifery Research Centre (MMRC). Over the course of her undergraduate career, Shikha has found a great passion for research and is excited to further the knowledge she has gained thus far. Contact: gandhs15@mcmaster.ca.
Study Description: Over the last 25 years, the profession of midwifery has continued to grow rapidly throughout Canada. Research suggests that midwifery-led care has the potential to improve maternal/infant outcomes, improve client satisfaction and increase breastfeeding rates. The purpose of this scoping review was to identify the progress, strengths, gaps, priorities, and directions of midwifery research in the Canadian context to develop resources for registered midwives, midwifery researchers, professional associations, regulatory bodies, and funding agencies.
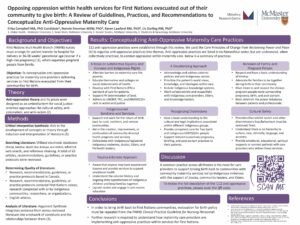
Erika Campbell
Poster Title: Opposing oppression within health services for First Nations evacuated out of their community to give birth: A Review of Guidelines, Practices, and Recommendations to Conceptualize Anti-Oppressive Maternity Care
Bio: Erika is a PhD candidate in Global Health at McMaster University. Her doctoral research, supervised by Dr. Liz Darling and Dr. Karen Lawford, explores the influence of the dominate western culture within the federal and Ontario healthcare systems related to the provision of maternity care provided to First Nations peoples who are evacuated out of their communities to give birth. She is unsure what she we do after completion of her PhD. However, Erika knows that she wants to contribute as a researcher, educator, and advocate to establishing and maintaining sexual and reproductive healthcare that is accessible and safe for service users.
Study Description: Using critical interpretive synthesis, Erika reviewed literature pertaining to guidelines, practices, and recommendations about maternity care for First Nations evacuated from their communities to give birth in hospitals to conceptualize anti-oppressive maternity care practices for care providers serving this patient population. Erika analyzed 63 different documents, from peer reviewed journal articles to gray literature, to thematically organize anti-oppressive practices through the Core Principles of Change of the Calls for Justice from Reclaiming Power and Place: The Final Report of the National Inquiry into Missing and Murdered Indigenous Women and Girls. This review is an ongoing piece of work that is likely to change in the way ideas are communicate, but Erika is grateful to be able to share this work to generate discussion about our collective responsibility to make maternity care anti-oppressive. Erika would like to acknowledge and thank her PhD committee, Dr. Liz Darling, Dr. Bonnie Freeman, and Dr. Karen Lawford, for their insights and feedback throughout the process of conducting this review.


