
THANK YOU!
Thank you to all the all the presenters, panelists, and attendees for such a successful symposium!
If you haven’t already, please complete the feedback survey so we can continue improving on making this a great experience for all. Thanks again to all those who helped make last week’s research symposium so enjoyable.
For those who were unable to attend or would like to watch the presentations again, recordings are now available below!
– –
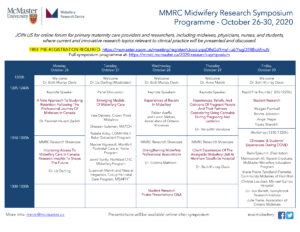
The McMaster Midwifery Research Centre is excited to announce the 2020 McMaster Midwifery Research Symposium will run over the course of October 26-30, 2020!
This year’s online format will be hosted from 12-1/1:30pm each day and will include panel discussions, keynote presentations, workshops and research rapid fire presentations for trainees. Tune in to learn about many topics impacting Canadian midwifery, pregnancy outcomes, and models of care.
Symposium Programme
Post-Symposium Feedback: Please help us improve the symposium for next year by providing your feedback. The survey is anonymous, unless you indicate your email address for the purpose of receiving a Symposium Certificate of Attendance that will be emailed to you. Provide your feedback here.
Recorded Sessions
|
MMRC-MidwiferyResearchSymposium-Keynote-FarimahZadeh-MidwiferyRetentionStudy-26Oct2020 |
Dr. Farimah Hakem Zadeh
A New Approach To Studying Retention: Following The Professional Journey Of Midwives In CanadaMonday, October 26, 2020 – 1200h Keynote Description: Funded by the Canadian Institutes of Health Research, the Canadian Midwifery Study is a multidisciplinary mixed-method research project led by Drs Lobb and Zeytinoglu, with Drs Neiterman and Zadeh as co-investigators. The research team also has Johanna Geraci from the College of Midwives of Ontario and a graduate of the McMaster Midwifery Education Programme on board. The vision of this project is to join forces with educators and policymakers to enhance midwives’ experiences throughout their career trajectory, from early professional training to later in their midwifery practice. The end goal of this project is to retain midwives in this profession which in turn would ensure a platform of high quality and accessible primary care for women in Canada. Project website: https://canadianmidwiferystudy.ca/. |
|
MMRC_Symposium-Keynote-Aseffa&Mehari-ExperiencesOfRacismInMW-28Oct2020-online |
Feben Aseffa, Director, Healthcare Equity, Quality and Human Rights, Association of Ontario Midwives Lwam Mehari, Association of Ontario Midwives Experiences Of Racism In Midwifery Wednesday, October 28, 2020 – 1200hLecture Description: Feben and Lwam will highlight findings from their research study: Experiences of Racism Among Ontario BIPOC Midwives and Students in Midwifery Education and Profession (2019). This study is the first Canadian study that investigated experiences of racism in midwifery, and it provided sobering findings of the impact of structural and interpersonal racism in both the midwifery education program and within the profession. The researchers have identified a substantial need for change, and the AOM Board of Directors have committed to working towards dismantling racism in the profession. The speakers will share some of the initiatives that have been undertaken to date to meet this goal. |
|
Keynote – Experiences, Beliefs, & Opinions of Pregnant People & Partners considering Cannabis during Pregnancy & Lactation |
Dr. Meredith Vanstone
The Experiences, Beliefs, And Opinions Of Pregnant People And Their Partners Considering Cannabis During Pregnancy And Lactation Thursday, October 29, 2020 – 1200h Lecture Description: Meredith will discuss a new CIHR-funded study she leads on decision-making about cannabis during pregnancy and lactation. Rates of cannabis use have been rising since recreational use was legalized in Canada, but evidence about the impacts of using cannabis during pregnancy and lactation is conflicting, weak, and in many cases absent. This presents a challenge for pregnant and lactating people who have compelling reasons to use cannabis, and clinicians who strive to encourage informed decisions that reduce risk. With an interprofessional team of collaborators including midwives, family physicians, and obstetricians, the team is conducting two systematic reviews about how pregnant people and their health care professionals understand the risks and benefits of cannabis use during pregnancy and lactation. After sharing some results from this review, Meredith will discuss the proposed next stages of the research: primary data collection from people who have decided to use (or stop using) cannabis during pregnancy or lactation and from prenatal health care providers who counsel pregnant people facing this decision. Project website: http://www.meredithvanstone.com/. |
|
Panel – Emerging Models of Midwifery Care |
Emerging Models of Midwifery Care Tuesday, October 27, 2020 at 1200hPanel Discussion: six highly innovative and recently implemented models of midwifery care in Canada will be discussed with the panelists who helped develop these models. Read more about the panelists and their models of care below. Facilitated by Dr. Liz Darling. |
|
Workshop – Clinicians’ & Students’ Experiences during COVID |
Clinicians’ & Students’ Experiences during COVID Friday, October 30, 2020 at 1230hWorkshop Discussion: five panelists discuss how the COVID-19 pandemic has drastically affected the provision of midwifery care, and how midwives, midwifery students, and midwifery clients have had to quickly adapt to continue to provide and receive the best quality of care possible. Facilitated by Remi Ejiwunmi. |
|
Showcase – Improving Access to MW Care in Canada |
Dr. Liz Darling
Improving Access to Midwifery Care in Canada: Research Insights to Shape the Future Monday, October 26, 2020 – 1240h Project Description: What do midwives need to know about how we can increase equitable access to midwifery care? This presentation will draw on findings from several research projects to synthesize key learnings related to improving access to midwifery care in the Ontario context, including, but not limited to content from the following research projects: Access to Midwifery Care and Low Socio-Economic Status; Value for Money: The Impact of Novel Alternate Funding Mechanisms for Midwifery Care; and Identifying Barriers and Facilitators to Midwives Mental Health. Project website: http://www.lizdarling.ca/. |
|
Showcase – Strengthening Midwifery Professional Associations |
Dr. Cristina Mattison
Strengthening Midwifery Professional Associations Wednesday, October 28, 2020 – 1240h Project Description: In collaboration with Kirsty Bourret, we are leading two CAM and Mitacs Accelerate-funded large, multi-country (Canada, Haiti, South Sudan, Democratic Republic of Congo, and Tanzania), mixed methods studies, focused on professional association strengthening and health professions education (healthcare skills transfer). We have developed evidence-informed theoretical frameworks to support programming designed to effectively strengthen midwifery associations and improve midwifery continuing education, to allow midwives to leverage the impact of their profession. Midwifery associations are an example of largely women led civil society organizations that play a critical role in improving sexual and reproductive health and rights and more broadly, achieving the Sustainable Development Goals. |
|
Showcase – Client Experiences of the Alongside Midwifery Unit at Markham Stouffville Hospital |
Dr. Beth Murray-Davis Project Description: How satisfied are clients who receive care on the Markham Stouffville Alongside Midwifery Unit (AMU)? What do they value about the care they receive? How does their experience compare to what they were expecting? This presentation will shed light on these questions. The presentation will focus on midwifery client experiences of receiving care at the AMU by sharing findings from a) survey results from those who gave birth on the AMU compared to those who gave birth prior to the opening of the unit, and b) in-depth interview responses from clients throughout the two years since the unit opened. Project website: https://mmrc.mcmaster.ca/research-topics/project/2018/10/10/evaluation-of-the-markham-stouffville-hospital-alongside-midwifery-unit-(msh-amu-evaluation), and, https://www.msh.on.ca/clinics-departments/stollery-family-centre-childbirth-children/alongside-midwifery-unit-amu. |
|
Student Research Poster – Q&A |
Student Research Poster Presentation Q&A Wednesday, October 28, 2020 – 1300hPoster Q&A: Graduate and undergraduate students working with Scientists at the McMaster Midwifery Research Centre present their research through posters. Posters are available below. |
|
Rapid Fire Rounds |
Rapid Fire Rounds
Friday, October 30, 2020 – 1200h Description: Four budding researchers present their work in 5 minutes each during this rapid fire rounds. Watch Meagan Furnivall, Bronte Johnston, Angel Najjar, and Touka Shamkhi to lear more about their research! Project descriptions and bios are available below. |
Speaker Bios & Lecture Descriptions
- Overview: Four leading researchers present their recent work on prescient topics for midwives.
 |
Dr. Farimah Hakem Zadeh
A New Approach To Studying Retention: Following The Professional Journey Of Midwives In CanadaMonday, October 26, 2020 – 1200h Keynote Description: Funded by the Canadian Institutes of Health Research, the Canadian Midwifery Study is a multidisciplinary mixed-method research project led by Drs Lobb and Zeytinoglu, with Drs Neiterman and Zadeh as co-investigators. The research team also has Johanna Geraci from the College of Midwives of Ontario and a graduate of the McMaster Midwifery Education Programme on board. The vision of this project is to join forces with educators and policymakers to enhance midwives’ experiences throughout their career trajectory, from early professional training to later in their midwifery practice. The end goal of this project is to retain midwives in this profession which in turn would ensure a platform of high quality and accessible primary care for women in Canada. Project website: https://canadianmidwiferystudy.ca/. Bio: Dr. Farimah Zadeh is an alumnus of McMaster University. Her expertise is in the area of evidence-based decision making, particularly applying it to enhancing the health of the health workforce. She is currently an assistant professor at York University, teaching Occupational Health and Safety and Organizational Development and Change courses. For the past seven years, Farimah has been a part of The Canadian Midwifery study research team. Contact: zadeh@yorku.ca, and Dr. Derek Lobb lobbd@mcmaster.ca. |

|
Feben Aseffa, Director, Healthcare Equity, Quality and Human Rights, Association of Ontario Midwives Lwam Mehari, Association of Ontario Midwives Experiences Of Racism In Midwifery Wednesday, October 28, 2020 – 1200hLecture Description: Feben and Lwam will highlight findings from their research study: Experiences of Racism Among Ontario BIPOC Midwives and Students in Midwifery Education and Profession (2019). This study is the first Canadian study that investigated experiences of racism in midwifery, and it provided sobering findings of the impact of structural and interpersonal racism in both the midwifery education program and within the profession. The researchers have identified a substantial need for change, and the AOM Board of Directors have committed to working towards dismantling racism in the profession. The speakers will share some of the initiatives that have been undertaken to date to meet this goal.Bio: Feben Aseffa is an alumni of the Ryerson University Midwifery Education Program and obtained a Master of Health Management from McMaster University. Since 2016 she has worked in the role of Quality and Risk Management Specialist at the Association of Ontario Midwives (AOM). Over the past 20 months, Feben has been leading initiatives to promote racial equity within midwifery, including leading the study: Experiences of Racism Among Ontario BIPOC Midwives and Students in Midwifery Education and Profession. She was recently appointed Director of Healthcare Equity, Quality and Human Rights at the AOM. Feben is committed to promoting and implementing evidence-based change management initiatives to address human rights-based inequities within midwifery and the healthcare system broadly. Contact: feben.aseffa@aom.on.ca. Bio: Lwam Mehari is an alumni of Western University’s Master of Public Health Program at the Schulich School for Medicine and Dentistry. She obtained her Honours Bachelor of Arts Degree from the University of Toronto in Bioethics and English. Lwam conducted Clinical Ethics research at Humber River Hospital in Toronto with a focus on racial equity, advance care planning and mental health. She completed her Master of Public Health practicum at the Association of Ontario Midwives and worked as a research assistant on the Experiences of Racism Among BIPOC Midwives and Students in Midwifery Education and Profession research study. Contact: lwam.mehari@aom.on.ca. |
 |
Dr. Meredith Vanstone
The Experiences, Beliefs, And Opinions Of Pregnant People And Their Partners Considering Cannabis During Pregnancy And Lactation Thursday, October 29, 2020 – 1200h Lecture Description: Meredith will discuss a new CIHR-funded study she leads on decision-making about cannabis during pregnancy and lactation. Rates of cannabis use have been rising since recreational use was legalized in Canada, but evidence about the impacts of using cannabis during pregnancy and lactation is conflicting, weak, and in many cases absent. This presents a challenge for pregnant and lactating people who have compelling reasons to use cannabis, and clinicians who strive to encourage informed decisions that reduce risk. With an interprofessional team of collaborators including midwives, family physicians, and obstetricians, the team is conducting two systematic reviews about how pregnant people and their health care professionals understand the risks and benefits of cannabis use during pregnancy and lactation. After sharing some results from this review, Meredith will discuss the proposed next stages of the research: primary data collection from people who have decided to use (or stop using) cannabis during pregnancy or lactation and from prenatal health care providers who counsel pregnant people facing this decision. Project website: http://www.meredithvanstone.com/. Bio: Dr. Meredith Vanstone is an Associate Professor in the Department of Family Medicine at McMaster University, a member of the Centre for Health Economics and Policy Analysis and an adjunct scientist of McMaster’s program for Education Research, Innovation and Theory. Her research examines the intersection of ethics and policy issues in primary care, specifically focusing on how people who lack power are affected by health policy and health professional practice. Contact: Meredith.vanstone@mcmaster.ca |
- Overview: Six highly innovative and recently implemented models of midwifery care in Canada will be discussed with the panelists who helped develop these models. Facilitated by Dr. Liz Darling.
 |
Kate Demers
Model of Care: Crown Point Midwives offer a variety of expanded midwifery services including contraception counselling including IUD insertions, medication abortions, STI screening and treatment and menopause information sessions. The focus is on reducing barriers to care with midwives offering services in Arabic, English, and French, with short wait times and within an interprofessional model. Program website: https://www.crownpointfhc.ca/midwives-new. Bio: Kate Demers is an assistant professor at McMaster University and practicing midwife at Community Midwives of Hamilton. She graduated from the McMaster Midwifery Education Program (MEP) in 2009. She also holds a BSc from McMaster University and MMid from the University of Sheffield. She is the lead midwife at Crown Point Midwives, an expanded midwifery care model practice in Hamilton. Her interests include improving access to sexual and reproductive health services, task sharing and expanded midwifery models. Contact: kdemers@mcmaster.ca. |
 |
Shezeen Suleman
Model of Care: MATCH – Midwifery and Toronto Community Health – is an innovative model of perinatal care based out of the South Riverdale Community Health Centre in East Toronto. The MATCH team is positioned within the primary health care team at the CHC. The team offers a wide variety of services, with a focus on full-spectrum perinatal care including pregnancy, labour, and birth, as well as postpartum care for infants and adults, well-gynecological care, pregnancy options counselling, medication abortion and early pregnancy loss management. The MATCH team is made up of four midwives and a social worker. The team also works closely with family doctors, nurse practitioners, registered nurses, dieticians, physiotherapists and harm reduction workers at the CHC to provide wrap-around services to its clients.Program website: https://www.srchc.ca/programs/family-programs/match-midwifery-and-toronto-community-health/. Bio: Shezeen Suleman (she/her) is a Registered Midwife in Toronto who graduated from Ryerson’s Midwifery Education Program in 2011. Prior to midwifery, she worked for a number years with immigrant youth and their families in the city in a variety of capacities. Now one of the co-lead midwives at MATCH (Midwifery and Toronto Community Health) at the South Riverdale Community Health Centre, she brings together her passion for work rooted in community to the provision of perinatal care for people living in East Toronto who otherwise have barriers to accessing high quality healthcare. Contact: ssuleman@srchc.com. |
 |
Natalie Kirby
Model of Care: Working Together to Lead Together: A Midwife-Led Well-Baby Outpatient Clinic: The CGMH Well-Baby Outpatient program is a midwife-led hospital outpatient clinic designed to improve access to essential maternal-child services by putting patients first and connecting families with appropriate, high-quality, evidence-based care. This new and innovative interdisciplinary model of care facilitates midwives to expand provision of service outside the current model of care in Ontario. The program targets specific community needs and has increased supports and resources for the community and improved care through collaboration. Program website: www.healthybabieshappyfamilies.ca. Bio: Natalie Kirby has been practicing midwifery since graduating from the MEP in 2009. Over the years, Natalie has become a Lactation Consultant as well as completed a Master’s in Health Science Education. Natalie is passionate about collaborative care and is the Clinic Lead for the interdisciplinary expanded care midwifery model, a well-baby outpatient clinic partnered with Collingwood General and Marine Hospital. It is a privilege and career highlight to explore innovative models of care that benefit the community, the clients and the care providers. Contact: kirbyn@cgmh.on.ca. |
 |
Maxine Vigneault
Model of Care: The Montfort Postnatal Care at Home Program provides the option of midwifery care for the first postpartum week to low-risk parent/infant dyads followed by an obstetrician/pediatrician or a family physician. Key components include: a prenatal info session aimed at preparing families for breastfeeding, newborn care and the transition from hospital to home, early discharge from hospital between 6 and 24 hours of a vaginal birth and within 24 hours of a caesarean birth, delivery of dyad-centered care via 2-3 home visits and telephone support and 24/7 on call coverage. https://hopitalmontfort.com/en/postnatal-homecare. Bio: Maxine Vigneault holds a BHSc in Midwifery from Laurentian University and has been a practicing midwife since 2007. She currently works as a registered midwife within the Montfort Postnatal Care at Home Program, having been involved in both its design and implementation. She was a former Head Midwife at the Montfort Hospital and Lead Midwife at the Ottawa Birth and Wellness Centre. Her interests lie in the integration of midwifery and access to midwifery care within interdisciplinary models. Contact: maxine.vigneault@gmail.com. |
 |
Jenni Huntly
Model of Care: The Midwifery Program at NorWest CHC was created to address current gaps in perinatal care that are impacting more marginalized, and vulnerable populations in Northwestern Ontario. The midwifery program provides prenatal and postpartum care to pregnant people who are clients of the CHC or in identified higher-risk social situations, group prenatal care and postpartum education groups, reproductive health counselling and contraceptive , and collaborative care with allied services in the CHC’s such as community health workers, counselling, substance involvement, smoking cessation etc. The program also provides postpartum and newborn care for 6 months after birth for people in the community without primary care providers. Program website: https://norwestchc.org/. Bio: Jenni Huntly (She/her) is a Registered Midwife with NorWest Community Health Centres in Thunder Bay, Ontario. Jenni has worked as a midwife in Quebec and Texas, as well as in Ontario and in Haiti. Passionate about culturally congruent care for all birthing people, including those in the 2SLGBTQIA+ community, Jenni has presented at various North American conferences, primarily on queer health issues and reproductive health access, and has trained hospital staff as well as midwifery students and doulas in various settings. She has been published as a contributing author of sexual health curricula (Center for Sex Education, 2020) and on various Clinical Practice Guidelines published by the Association of Ontario Midwives (2012 – 2016). She has the amazing support of her queer blended family for her midwifery and advocacy work. Contact: jhuntly@norwestchc.org. |

|
Susannah Merritt & Natalie Tregaskiss
Model of Care: Susannah Merritt and Natalie Tregaskiss are the coordinators of the Group Perinatal Care (GPC) Program at the Mount Sinai Academic Family Health Team (MSAFHT). They are fully integrated into a team that includes family physicians, residents, nurses, nurse practitioners, pharmacist, social workers, and dietitians. In this midwifery-led GPC model, prenatal care alternates between group visits (facilitated by midwife and resident) and individual clinic visits with the staff physician. During the group sessions, the midwives and family medicine residents provide one-on-one pregnancy care through a ‘belly check’ and facilitate the group discussions which educate pregnant people and their support people about pregnancy, birth, and the immediate first 6-weeks postpartum. The midwife has a supervisory role and is instrumental in the evaluation and teaching of medical residents. The birth is attended by the Family Medicine obstetrics team. The midwives provide post-partum home visiting (ideally the initial newborn visit) to support breastfeeding and postpartum transitioning. Group sessions continue into the postpartum period with a focus on transition to parenthood and infant development. Program website: https://www.afhto.ca/d3-evaluation-midwifery-led-group-perinatal-care-academic-family-health-team. Susannah Merritt: Susannah Merritt graduated with honors from the Ryerson Midwifery Program in 2010 and has been practicing in the GTA since. Prior to midwifery, Susannah completed an undergraduate degree in English and International Relations at the University of Toronto. As one of the Group Prenatal Care Coordinators at the Mount Sinai Academic Family Health Team, Susannah contributes to ongoing program evaluation and has presented at the Family Medicine Forum (FMF) 2016, The Academic Family Health Teams of Ontario Conference (AFHTO) 2019 and the Granovsky Gluskin Family Medicine Conference (GGFMC) 2020. Susannah is a member of the Baby Friendly Initiative (BFI) committee at Mount Sinai Hospital and contributes to breastfeeding policy development and education. Susannah Lives in Toronto with her two young children. Contact: Susannah.merritt@sinaihealth.ca Natalie Tregaskiss: Natalie Tregaskiss worked as a Labour and Delivery nurse for five years before pursuing a career in midwifery. She was the first graduate from the Post –Baccalaureate Program for Health Professionals and obtained her Bachelor of Health Sciences in Midwifery (with honours) from Ryerson University in 2011. Natalie has been the Group Perinatal Care Coordinator at the Mount Sinai Academic Family Health Team since its inception in 2016 and continues to practice as a Labour and Delivery nurse at St. Michael’s hospital in downtown Toronto. Natalie participates in ongoing evaluation of the GPC program and has presented preliminary results at the Academic Family Health Teams of Ontario 2019 Conference and the Granofsky Gluskin Family Medicine Conference 2020. Natalie is the chair of the Group Perinatal Care Committee and participates in the Family Medicine Maternity Care Committee and the Baby Friendly Initiative Committee at Mount Sinai Hospital. She is currently pursuing her lactation consultant certification and lives in the Kensington Market area of Toronto with her three kids. Contact: natalie.tregaskiss@sinaihealth.ca. |
- Overview: Five panelists and a facilitator will discuss how the COVID-19 pandemic has drastically affected the provision of midwifery care, and how midwives, midwifery students, and midwifery clients have had to quickly adapt to continue to provide and receive the best quality of care possible.
- For those attending the panel workshop “Clinicians’ & Students’ Experiences During COVID” on Friday, October 30, 1230-1330h: In order to give some space for creating a synergy of ideas and dialogue during these challenging times, please consider submitting your questions and comments in advance to the workshop panelists through this Advance Questions & Comments form. Responses are anonymous and will be collated and summarized for the workshop facilitator to present to the panel. Post your questions here.
 |
Remi Ejiwunmi
Bio: Remi Ejiwunmi, MSc, RM, and facilitator for symposium workshop on “Clinicians’ & Students’ Experiences During COVID”, is a practicing midwife in Mississauga, Ontario, and Head of the Division of Midwifery at Trillium Health Partners. Remi’s research interests include quality improvement, patient-centred care, and system thinking. Remi currently sits at a Board Member at HIROC and is a member of the AOMs Quality Insurance and Risk Management committee. She also helped lead the development of Perinatal Quality and Practice Councils at her hospital, Trillium Health Partners. Remi was part of the interdisciplinary team at PCMCH that developed the Maternal Newborn Guidelines for COVID earlier this year. Remi was President at the Association of Ontario Midwives (AOM) from 2001 to 2004. Contact: rejiwunmi@midwivesofmississauga.ca. |
 |
Christie Lockhart Bio: A graduate of McMaster University’s Midwifery Education Program, Christie Lockhart is the Chief of the Department of Midwifery and Co-Program Medical Director of Maternal Newborn & Child Health Service at Michael Garron Hospital. Christie has been a practicing midwife in Toronto since 2007 and is a practice partner at The Midwives’ Clinic of East York-Don Mills. Christie is a clinical preceptor and Adjunct Professor at Ryerson University in the Midwifery Education Program, as well as a member of Ryerson’s Midwifery Education Program Advisory Council. Christie has previously been a member of the BORN Midwifery Advisory Committee and the AOM Board of Directors. Contact: christie.lockhart@tehn.ca |
 |
Dr. Jon Barrett
Bio: Dr. Jon Barrett, MBBch, MD, FRCOG, FRCSC, is the Chief of Maternal Fetal Medicine at Sunnybrook Health Sciences Centre and a Professor of Obstetrics and Gynecology at the University of Toronto. He is a Senior Scientist at the Sunnybrook research Institute and the Program Research Director of the Women and Babies Program. He is the medical co-director of Clinical Trial Services at Sunnybrook Health Sciences Centre and holds the Waks Family Research Chair of Maternal Fetal Medicine Research. He is a World Health Organization advisor on Maternal Health, Vice Chair of the Board of the Society of Obstetricians and Gynaecologists and the International Society of Twin Research, and President of the Canadian Society of Maternal Fetal Medicine. He is the Founder and Chair of the Southern Ontario Obstetrical Network (SOON). He has recently been appointed Vice Chair Quality for the Department of Obstetrics, University of Toronto. He has held more than $20 million in grants, most prominently in the conduct of randomized controlled trials, wherein he has obtained international recognition in the field of multiple pregnancy. More recently his research has been channeled to both improving outcomes and preventing the occurrence of preterm birth via population interventions. His most recent and ongoing initiative has been the formation the Alliance for the prevention of preterm and stillbirth in Ontario, which is enjoying increasing philanthropic and ministry support. Program: https://sunnybrook.ca/research/. Contact: jon.barrett@sunnybrook.ca. |
 |
Julie Toole
Bio: Julie Toole, BA, BHSc, MHSc, RM, is a Quality & Risk Management Specialist with the Association of Ontario Midwives (AOM), focusing on management of adverse events, privacy, ethics, workplace bullying and mental health. She is the association’s project lead on COVID-19 work which is supported by her experience in pandemic and outbreak monitoring. Her experience considers how the AOM mobilized and mounted a thorough communication and membership support strategy during COVID. Julie also provides significant contribution to clinical ethics work at the AOM as the lead of two ethics task forces, and is passionate about supporting midwives in the provision of quality, safe and ethical midwifery care. Julie completed a Master of Health Sciences degree in Medical Sciences, Bioethics at the University of Toronto and a Bachelor of Health Sciences in Midwifery at Ryerson University. Program: https://www.ontariomidwives.ca/staff-directory. Contact: julie.toole@aom.on.ca. |
 |
Maimoonah Ali
Bio: Maimoonah Ali is an Eritrean-Canadian midwife born and raised in Toronto. She is a recent graduate of the Midwifery Education Program at McMaster University. She spent her senior year finishing training at the Community Midwives of Hamilton and has completed placements in Winnipeg and throughout southern Ontario. Maimoonah is currently practicing in Toronto at Midwifery Care – North Don River Valley. Contact: maimoonah8629@gmail.com. |
 |
Marie-Pierre Tendland-Frenette
Bio: Marie-Pierre Tendland-Frenette holds a BSc in Biology with a specialization in Microbiology (University of Waterloo, 2009), and a BHSc in Midwifery (McMaster University, 2013). Marie-Pierre is a fluent French speaker, and works off-site providing Midwifery care at Centre de Santé Communautaire. In addition to her work as a Registered Midwife, Marie-Pierre is a member of the Maternal Quality of Care Committee at St Joseph’s Healthcare Hamilton and is a part of the Association of Ontario Midwives (AOM) Hyperbilirubinemia Work Group. Marie-Pierre also teaches as a clinical preceptor to students in our clinic. Contact: mptendlandfrenette@gmail.com |
- Overview: Three midwifery research scholars will present their work on a variety of topics, approaches, and methods highlighting research being done at the McMaster Midwifery Research Centre.
 |
Dr. Liz Darling Improving Access to Midwifery Care in Canada: Research Insights to Shape the Future Monday, October 26, 2020 – 1240h Bio: Dr. Liz Darling, BArtsSc, BHSc, MSc, PhD, is a Registered Midwife, Assistant Dean and Director of the Midwifery Education Program, Associate Professor in the Department of Obstetrics and Gynecology, an Adjunct Scientist at the Institute for Clinical Evaluative Sciences, and an Associate with the Department of Health Research Methods, Evidence, and Impact at McMaster University. She is the principal investigator on a CIHR Early Career Operating Grant in Maternal, Reproductive, Child, and Youth Health. Her current research interests include: the organization of midwifery services, health disparities, access to care, health policy, and perinatal health surveillance. She conducts mixed methods research and has particular expertise in the midwifery data collected in Ontario’s perinatal registry (BORN-Ontario). Contact: darlinek@mcmaster.ca Project Description: What do midwives need to know about how we can increase equitable access to midwifery care? This presentation will draw on findings from several research projects to synthesize key learnings related to improving access to midwifery care in the Ontario context, including, but not limited to content from the following research projects: Access to Midwifery Care and Low Socio-Economic Status; Value for Money: The Impact of Novel Alternate Funding Mechanisms for Midwifery Care; and Identifying Barriers and Facilitators to Midwives Mental Health. Project website: http://www.lizdarling.ca/. |
 |
Dr. Cristina Mattison
Strengthening Midwifery Professional Associations Wednesday, October 28 – 1240h Bio: Dr. Cristina A. Mattison is an Assistant Professor (Part-time), Department of Health Research Methods, Evidence, and Impact. Cristina obtained her PhD in Health Policy and MSc in Global Health from McMaster University. In her former role as a Scientific Lead, Stakeholder Engagement and Systems Analysis at the McMaster Health Forum, Cristina oversaw the scientific aspects of and leading the execution of evidence syntheses and the Health Systems Learning training program for policymakers and health-system managers. Currently, Cristina is a fellow at the MMRC focusing her work on understanding the integration of midwifery into health systems in Canada. In addition, Cristina is working with the Canadian Association of Midwives (CAM) to develop two conceptual frameworks related to healthcare skills transfer and civil society strengthening to inform the monitoring and evaluation of CAM’s global programs. Contact: mattisc@mcmaster.ca. Project Description: In collaboration with Kirsty Bourret, we are leading two CAM and Mitacs Accelerate-funded large, multi-country (Canada, Haiti, South Sudan, Democratic Republic of Congo, and Tanzania), mixed methods studies, focused on professional association strengthening and health professions education (healthcare skills transfer). We have developed evidence-informed theoretical frameworks to support programming designed to effectively strengthen midwifery associations and improve midwifery continuing education, to allow midwives to leverage the impact of their profession. Midwifery associations are an example of largely women led civil society organizations that play a critical role in improving sexual and reproductive health and rights and more broadly, achieving the Sustainable Development Goals. |
 |
Dr. Beth Murray-Davis Client Experiences Of The Alongside Midwifery Unit At Markham Stouffville Hospital Thursday, October 29 – 1240hBio: Dr. Beth Murray-Davis, BA, BHSc, MA, PhD, RM, is an Associate Professor in the Midwifery Education Program and Department of Obstetrics and Gynecology. She is a co-PI for a CIHR Clinician Investigator Team Grant examining Non-Communicable Diseases in Obstetrics. Her current research interests include pregnant peoples’ experiences of healthy nutrition and exercise during pregnancy and postpartum, fetal movement awareness, midwifery experiences of caring for complicated pregnancies, client and health care provider experiences of alternative models of practice for midwives, and client decision making about place of birth. Dr. Murray-Davis has worked as a midwife in Hamilton since 2003. Contact: bmurray@mcmaster.ca.Project Description: How satisfied are clients who receive care on the Markham Stouffville Alongside Midwifery Unit (AMU)? What do they value about the care they receive? How does their experience compare to what they were expecting? This presentation will shed light on these questions. The presentation will focus on midwifery client experiences of receiving care at the AMU by sharing findings from a) survey results from those who gave birth on the AMU compared to those who gave birth prior to the opening of the unit, and b) in-depth interview responses from clients throughout the two years since the unit opened. Project website: https://mmrc.mcmaster.ca/research-topics/project/2018/10/10/evaluation-of-the-markham-stouffville-hospital-alongside-midwifery-unit-(msh-amu-evaluation), and, https://www.msh.on.ca/clinics-departments/stollery-family-centre-childbirth-children/alongside-midwifery-unit-amu. |
- Overview: Graduate and undergraduate students working with Scientists at the McMaster Midwifery Research Centre present their research through posters available online during the symposium for your review at https://mmrc.mcmaster.ca/2020-research-symposium.
- Please join us via Zoom for a Q&A with poster presenters, immediately following Dr. Cristina Mattison’s MMRC Research Showcase “Strengthening Midwifery Professional Associations”.
| Efrah Yousuf
Bio: Efrah Yousuf is currently completing a PhD in Medical Sciences at McMaster University, under the supervision of Dr. Katherine Morrison (Department of Pediatrics). She obtained her BSc (Honours) degree in Bio-Medical Science from the University of Guelph. Her research is centred on exploring the gut microbiota development of infants born preterm compared to infants born full term. Contact: yousufei@mcmaster.ca. Study Description: Probiotics, which are comprised of live microorganisms that often belong to the bacterial groups Bifidobacterium and Lactobacillus, are becoming a prevalent supplement to prevent necrotizing enterocolitis in infants born preterm. However, little is known about the ability of these supplements to colonize the gut or how they affect endogenous bacterial strains and the overall gut community. In this study, we compared the prevalence and abundance of Bifidobacterium and Lactobacillus in the gut of preterm infants who were and were not exposed to a probiotic supplement in-hospital. A higher abundance of suspected probiotic bifidobacteria was found in probiotic-exposed infants out to 5 months corrected age. Further research is needed to fully discriminate probiotic bacterial strains from endogenous strains and to understand their impact on infant health. |
 |
Chiara-Maria Homann
Bio: Chiara-Maria Homann recently graduated from the MSc Medical Science program at McMaster University, after completing her BSc in Nutritional Science at the Technical University of Munich. During her master’s studies she focused on the influence nutritional choices have on the developing gut microbiome in healthy, full-term infants, which were under the supervision of midwives. Contact: homannc@mcmaster.ca. Study Description: The introduction of solid foods is an important dietary event during infancy that causes dramatic shifts in gut microbial composition contributing to a more adult-like state. Infant gut bacterial dynamics, especially in relation to nutritional intake remain understudied. In this study, stool samples and food diaries were collected daily for two weeks surrounding the introduction of solid foods allowing for longitudinal analysis of the changes occurring at this time. This study furthers our understanding of a factor that impacts the gut microbiome in early life before the adult-like microbiota is attained at around three years of age. |
 |
Malaak Angel Najjar
Bio: Malaak Angel Najjar is a recent graduate of the MSc Global Health program at McMaster. During both her master’s and undergraduate studies in Biology and Biostatistics, she pursued a research focus on neonatal health and obstetric care in low- and middle-income countries. As a global health student, midwifery practice around the world became an important facet of this research. She nurtures a keen interest in improving neonatal mortality rates through midwifery education, including regulatory policy and training programs. Contact: najjam1@mcmaster.ca Study Description: Annually, there are 2.7 million neonatal deaths and an additional 2.6 million stillbirths across the globe; 90% of which occur in low- and middle-income countries. Training programs, such as Helping Babies Breathe, are implemented for midwives and other skilled birth attendants in hopes of improving outcomes for mothers and their newborns. To quantify the neonatal health impact of midwifery training, this review explores how various continuing education training programs impact clinical health outcomes in the early neonatal period. |
 |
Maisha Ahmed
Bio: Maisha Ahmed is a second year midwifery student at McMaster University, who worked as a Research Assistant with the Summer Studentship Award at the McMaster Midwifery Research Centre. Before starting midwifery, she studied at McMaster University in the (Honours) Integrated Sciences program for two years, where she found her passion in research. Contact: ahmedm82@mcmaster.ca. Study Description: The Markham Stouffville Hospital Alongside Midwifery Unit (MSH AMU) is the first of its kind in Canada and designed using existing evidence on the influences of the built environment on birth outcomes. The MSH AMU uses the aesthetics of the space and availability of birth tools to encourage physiologic labour and birth. The purpose of this mixed-methods study is to assess the impacts the environment of the MSH AMU has on the experiences of clients and midwives. Findings from this study can inform future innovations in Ontario midwifery care when designing healthcare facilities. |
 |
Aisha Jansen
Bio: Aisha Jansen is a second year midwifery student at McMaster University, where she is currently working as a Research Assistant with the McMaster Midwifery Research Centre. Before coming to McMaster, she completed her BSc (Honours) in Life Sciences at Queen’s University with a specialization in Biomedical Science. Her fourth year thesis at Queen’s centred around the use of ultrasound grayscale ranges to determine carotid plaque composition. Contact: jansea1@mcmaster.ca. Study Description: Midwifery care has the potential to improve access to health care for underserved populations (e.g. those at risk of poor access to health care and poor health outcomes). We hypothesize that midwifery services that target the unique needs of underserved populations have the potential to save the health system money, but this has not yet been demonstrated through research. This scoping review aims to synthesize previous approaches to economic analyses of interventions targeting underserved pregnant people and new parents. The results of this review will inform the development of an economic analysis framework that can be applied to expanded midwifery care models serving underserved populations. |
 |
Abdullah Haroon
Study Description: Limited healthcare provider knowledge and negative attitudes towards family planning and abortion care are factors implicated in the high level of unsafe abortions and the low level of contraceptive uptake in Pakistan. To address these gaps, an interactive eBook targeted for midwives in Pakistan was developed. This eBook uses an innovative design to provide comprehensive information pertinent to family planning methods, post-abortion care, and counseling approaches in a culturally sensitive manner. It also provides 15 audios and 7 videos in Urdu to facilitate the understanding of complex concepts. A mixed methods approach was used to evaluate the eBook at pilot workshops in Pakistan. The feedback was overwhelmingly positive. Participants found the eBook’s design appealing and user-friendly, and its content easy to grasp and relevant to their practice. Bio: Abdullah Haroon is currently a second-year medical student at the University of Ottawa. He completed his undergraduate degree in the Bachelor of Health Sciences (Honours) program at McMaster University where he worked as a research assistant with the McMaster Midwifery Research Centre. He co-leads the Women’s Health Interest Group at uOttawa, a group that aims to educate medical students on the multifaceted nature of Women’s Health. Contact: Abdullah.Haroon@uottawa.ca. |
- Overview: Four budding researchers will present their work in 5 minutes each during this rapid fire rounds.
 |
Meagan Furnivall
Bio: Meagan Furnivall, BA, BHSc, RM, is a registered midwife working in London, and is completing her Master’s in Health Science Education at McMaster University. She has active ongoing research studies at London Health Sciences Centre collegially with other obstetricians and anesthesiologists. Some of her research interests include skin-to-skin contact in caesarean section, interprofessional collaboration, and exploring how to teach obstetrical residents and midwifery students how best to engage in decision-making with clients. Contact: furnivm@mcmaster.ca. Study Description: Shared Decision Making is considered a favourable method of decision making with patients for both obstetricians and midwives alike. There is minimal understanding in the literature as to how exactly midwifery students and obstetrical residents understand and learn this process. The results of this grounded theory |
 |
Bronte Johnston
Bio: Bronte Johnston graduated Summa Cum Laude from McMaster’s Bachelor of Health Sciences Program and is currently pursuing the Master of Health Sciences Education Program also at McMaster. She is a research fellow of the McMaster Midwifery Research Centre and holds membership at McMaster Education Research, Innovation and Theory program. Her research interests include improving maternal health outcomes and the expanding scope of midwifery through education. Bronte has received two Ontario Graduate Scholarships for her master’s thesis which is evaluating Point of Care Ultrasound training for midwives. Contact: johnsb11@mcmaster.ca. Study Description: In 2018, the College of Midwives of Ontario expanded the scope of practice for registered midwives to include performing point of care ultrasound (POCUS) -which can aid an obstetric clinical exam. This study explores the first Ontario POCUS curriculum for midwives and evaluates learners’ skills, knowledge, and behaviours using quantitative and qualitative data. The results illustrate how midwives learn POCUS, how they are integrating it within their practices and the expanding scope of midwifery. https://www.normanresearchday.ca/wipcurricula |
 |
Malaak Angel Najjar
Bio: Malaak Angel Najjar is a recent graduate of the MSc Global Health program at McMaster. During both her master’s and undergraduate studies in Biology and Biostatistics, she pursued a research focus on neonatal health and obstetric care in low- and middle-income countries. As a global health student, midwifery practice around the world became an important facet of this research. She nurtures a keen interest in improving neonatal mortality rates through midwifery education, including regulatory policy and training programs. Contact: najjam1@mcmaster.ca. Study Description: The Peer-to-Peer Midwifery Program is an international initiative connecting undergraduate students from Ontario and Southern Australia. This program aims to dismantle barriers in sociocultural understanding and improve the scope of global health knowledge of midwifery students through reflective educational practice. By providing students with the opportunity to connect with other like-minded individuals through an online social platform, their knowledge of midwifery and global health is expected to expand. Although pen-pal style programs for undergraduates are seldom reported in the literature, evidence suggests that student reflection and understanding is facilitated when international collaboration is included in the form of a learning companion to communicate with. Especially during a time when learning is becoming more virtual, these connections are more important than ever before. |
 |
Touka Shamkhi
Bio: Touka Shamkhi is a midwifery student at McMaster and the primary investigator for this research project. Her research interests include equity in the midwifery education program and profession, and addressing racialized health disparities. Touka is the 2019 recipient of the HIROC Just Culture and Patient Safety Culture Award for her work on this research project and effort in addressing inequities in maternity care. Contact: shamkhit@mcmaster.ca. Study Description: This study explores resilience as it is described and experienced by racialized midwifery students in Ontario. Racialized midwifery students experience resilience differently than their non-racialized peers largely due to the ways in which racism and systemic whiteness/white supremacy colours their experiences in the MEP. In order to increase representation, retention and graduation of racialized students in midwifery, study findings will be used to move towards a more just midwifery culture that addresses and tackles its systemic whiteness. |
Student Research Posters
Student Research Posters are available all week for symposium attendees to read through. Study description and presenter bios are available below. Poster Presenters will be available for a Question & Answer period on October 28, 2020 at 13:00.
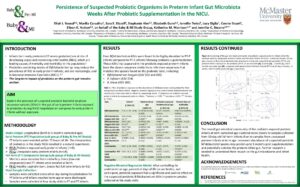
Efrah Yousuf
Study Description: Probiotics, which are comprised of live microorganisms that often belong to the bacterial groups Bifidobacterium and Lactobacillus, are becoming a prevalent supplement to prevent necrotizing enterocolitis in infants born preterm. However, little is known about the ability of these supplements to colonize the gut or how they affect endogenous bacterial strains and the overall gut community. In this study, we compared the prevalence and abundance of Bifidobacterium and Lactobacillus in the gut of preterm infants who were and were not exposed to a probiotic supplement in-hospital. A higher abundance of suspected probiotic bifidobacteria was found in probiotic-exposed infants out to 5 months corrected age. Further research is needed to fully discriminate probiotic bacterial strains from endogenous strains and to understand their impact on infant health.
Chiara-Maria Homann
Study Description: The introduction of solid foods is an important dietary event during infancy that causes dramatic shifts in gut microbial composition contributing to a more adult-like state. Infant gut bacterial dynamics, especially in relation to nutritional intake remain understudied. In this study, stool samples and food diaries were collected daily for two weeks surrounding the introduction of solid foods allowing for longitudinal analysis of the changes occurring at this time. This study furthers our understanding of a factor that impacts the gut microbiome in early life before the adult-like microbiota is attained at around three years of age.
Malaak Angel Najjar
Study Description: Annually, there are 2.7 million neonatal deaths and an additional 2.6 million stillbirths across the globe; 90% of which occur in low- and middle-income countries. Training programs, such as Helping Babies Breathe, are implemented for midwives and other skilled birth attendants in hopes of improving outcomes for mothers and their newborns. To quantify the neonatal health impact of midwifery training, this review explores how various continuing education training programs impact clinical health outcomes in the early neonatal period.
Maisha Ahmed
Study Description: The Markham Stouffville Hospital Alongside Midwifery Unit (MSH AMU) is the first of its kind in Canada and designed using existing evidence on the influences of the built environment on birth outcomes. The MSH AMU uses the aesthetics of the space and availability of birth tools to encourage physiologic labour and birth. The purpose of this mixed-methods study is to assess the impacts the environment of the MSH AMU has on the experiences of clients and midwives. Findings from this study can inform future innovations in Ontario midwifery care when designing healthcare facilities.
Aisha Jansen
Study Description: Midwifery care has the potential to improve access to health care for underserved populations (e.g. those at risk of poor access to health care and poor health outcomes). We hypothesize that midwifery services that target the unique needs of underserved populations have the potential to save the health system money, but this has not yet been demonstrated through research. This scoping review aims to synthesize previous approaches to economic analyses of interventions targeting underserved pregnant people and new parents. The results of this review will inform the development of an economic analysis framework that can be applied to expanded midwifery care models serving underserved populations.
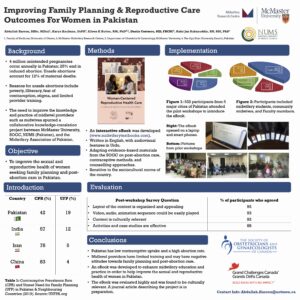
Abudullah Haroon
Study Description: Limited healthcare provider knowledge and negative attitudes towards family planning and abortion care are factors implicated in the high level of unsafe abortions and the low level of contraceptive uptake in Pakistan. To address these gaps, an interactive eBook targeted for midwives in Pakistan was developed. This eBook uses an innovative design to provide comprehensive information pertinent to family planning methods, post-abortion care, and counseling approaches in a culturally sensitive manner. It also provides 15 audios and 7 videos in Urdu to facilitate the understanding of complex concepts. A mixed methods approach was used to evaluate the eBook at pilot workshops in Pakistan. The feedback was overwhelmingly positive. Participants found the eBook’s design appealing and user-friendly, and its content easy to grasp and relevant to their practice.


